The Connection Between Eating Disorders and Suicide Risk
The Connection Between Eating Disorders and Suicide Risk
Discover the intricate connection between eating disorders and suicide risk in this comprehensive blog. Learn about the underlying factors, warning signs, and strategies for prevention and intervention to promote mental health and well-being.
Introduction:
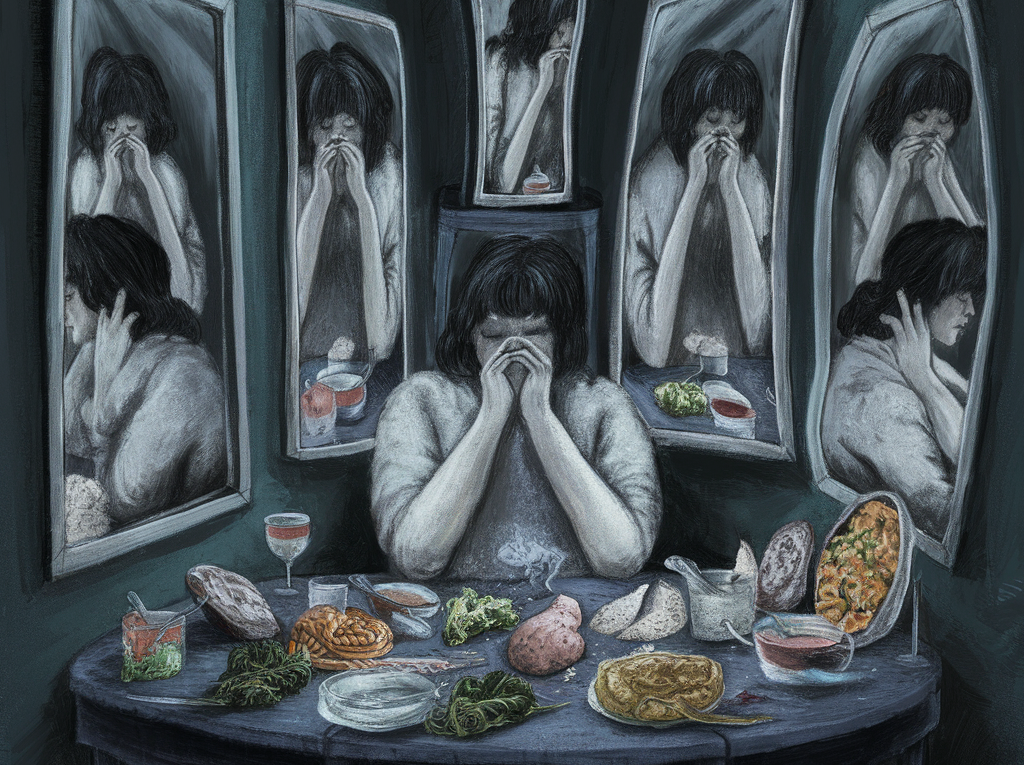
Eating disorders are pervasive and intricate mental health conditions that exert a profound impact on individuals worldwide, encompassing various age groups, genders, and socioeconomic backgrounds. These disorders, including anorexia nervosa, bulimia nervosa, and binge-eating disorder, are characterized by abnormal eating behaviors, distorted body image, and an overwhelming preoccupation with weight and shape. While the physical health implications of eating disorders, such as malnutrition and organ damage, have received considerable attention, their association with mental health issues, particularly suicide risk, remains relatively understudied and underreported.
The prevalence of eating disorders is alarmingly high, affecting millions of individuals globally and leading to significant morbidity and mortality rates. Despite advancements in research and treatment modalities, the societal stigma surrounding mental health conditions often perpetuates misconceptions and barriers to care for those struggling with eating disorders. Consequently, many individuals may suffer in silence, grappling with the debilitating effects of their condition without adequate support or intervention.
In this comprehensive blog, we embark on a journey to delve into the intricate connection between eating disorders and suicide risk. By shedding light on the underlying factors, warning signs, and strategies for prevention and intervention, we aim to increase awareness and understanding of this critical issue. Through comprehensive exploration and analysis, we endeavor to provide valuable insights and resources to support individuals affected by eating disorders and mitigate the devastating consequences of suicide within this vulnerable population.

Throughout this blog, we will navigate the complex interplay between eating disorders and suicide risk, examining the multifaceted factors that contribute to heightened vulnerability. From exploring the psychological and emotional toll of living with an eating disorder to understanding the societal pressures and cultural influences that exacerbate mental health challenges, we will uncover the intricate web of factors that underpin this relationship. Additionally, we will illuminate the warning signs and red flags indicative of suicide risk in individuals with eating disorders, empowering readers to recognize and respond to these concerns with compassion and urgency.
Furthermore, we will delve into the strategies and approaches for prevention and intervention, emphasizing the importance of early identification, comprehensive treatment, and supportive environments. By equipping readers with knowledge and resources, we aim to foster resilience, promote recovery, and ultimately save lives within the eating disorder community. Through collaborative efforts and collective advocacy, we can dismantle the barriers to care and create a more inclusive and compassionate society where individuals with eating disorders receive the support and understanding they deserve.
Join us on this enlightening journey as we navigate the complexities of eating disorders and suicide risk, striving to raise awareness, inspire action, and foster hope for a brighter future. Together, we can make a meaningful difference in the lives of those affected by these challenging and often misunderstood conditions, promoting mental health and well-being for all.
Understanding Eating Disorders:
Eating disorders are complex and debilitating psychiatric illnesses characterized by abnormal eating behaviors, distorted body image, and a profound fear of gaining weight or becoming fat. These conditions deeply affect individuals’ physical and psychological well-being, often leading to severe health complications and impairments in daily functioning. While there are various types of eating disorders, the most common include anorexia nervosa, bulimia nervosa, and binge-eating disorder, each presenting with distinct features and symptoms.

1. Anorexia Nervosa:
Anorexia nervosa is characterized by extreme dietary restriction and an intense preoccupation with maintaining a low body weight. Individuals with anorexia often perceive themselves as overweight, despite being significantly underweight, and engage in restrictive eating patterns to achieve their desired weight loss goals. Common behaviors associated with anorexia include severe calorie restriction, excessive exercise, and a distorted perception of body size and shape. Physical manifestations of anorexia may include emaciation, amenorrhea (absence of menstruation), and electrolyte imbalances.
2. Bulimia Nervosa:
Bulimia nervosa is characterized by recurrent episodes of binge eating followed by compensatory behaviors to prevent weight gain, such as self-induced vomiting, laxative abuse, or excessive exercise. Individuals with bulimia often experience feelings of guilt, shame, and loss of control during binge episodes, followed by a cycle of purging behaviors to alleviate distress. Unlike anorexia, individuals with bulimia may maintain a relatively normal body weight, making it harder to detect the disorder based on physical appearance alone.
3. Binge-Eating Disorder (BED):
Binge-eating disorder involves recurrent episodes of consuming large quantities of food in a short period, accompanied by a sense of loss of control and distress. Unlike bulimia, individuals with BED do not engage in compensatory behaviors such as purging, which can lead to significant weight gain and obesity-related health complications over time. Binge-eating episodes are often triggered by emotional distress or negative mood states, and individuals may experience feelings of guilt, shame, and embarrassment following these episodes.
The prevalence of eating disorders is alarmingly high, affecting millions of people worldwide across diverse demographic groups. While eating disorders are more commonly diagnosed in adolescence and early adulthood, they can occur at any age and affect individuals of all genders, ethnicities, and socioeconomic backgrounds. Research suggests that eating disorders disproportionately affect women, with females accounting for the majority of diagnosed cases. However, there is growing recognition of eating disorders among males and individuals across the gender spectrum, highlighting the need for gender-inclusive approaches to diagnosis and treatment.
The exact causes of eating disorders are multifactorial and complex, involving a combination of genetic, biological, psychological, and sociocultural factors. Genetic predisposition and familial history may increase an individual’s susceptibility to developing an eating disorder, while neurobiological factors such as imbalances in neurotransmitters like serotonin and dopamine may contribute to disordered eating behaviors. Additionally, psychological factors such as low self-esteem, perfectionism, and body dissatisfaction play a significant role in the development and maintenance of eating disorders.
Sociocultural influences, including societal pressures to attain unrealistic beauty standards, diet culture, and media portrayals of thinness, also contribute to the onset and perpetuation of eating disorders. These sociocultural factors can fuel body dissatisfaction and drive individuals to engage in disordered eating behaviors in pursuit of an unattainable ideal. Moreover, experiences of trauma, abuse, or interpersonal difficulties may increase vulnerability to developing eating disorders as maladaptive coping mechanisms for managing emotional distress.
In summary, eating disorders are complex mental health conditions characterized by abnormal eating behaviors, distorted body image, and intense fear of weight gain. While anorexia nervosa, bulimia nervosa, and binge-eating disorder are the most well-known types of eating disorders, other specified feeding or eating disorders (OSFED) and avoidant/restrictive food intake disorder (ARFID) also exist, each with its unique features and symptoms. The prevalence of eating disorders is high, affecting millions of individuals worldwide, and the exact causes are multifactorial, involving a combination of genetic, biological, psychological, and sociocultural factors. Recognizing the complexities of eating disorders is crucial for promoting early intervention, effective treatment, and long-term recovery for those affected by these debilitating conditions.
Understanding Suicide Risk:
Suicide represents a tragic and preventable loss of life, with millions of individuals worldwide succumbing to its devastating effects each year. Despite significant advancements in mental health awareness and suicide prevention efforts, the global prevalence of suicide remains alarmingly high, making it a leading cause of death across diverse demographic groups. While suicide is a complex phenomenon influenced by a multitude of factors, including mental illness, substance abuse, trauma, and interpersonal conflicts, individuals with eating disorders are particularly vulnerable to experiencing suicidal ideation and behavior.
Eating disorders, including anorexia nervosa, bulimia nervosa, and binge-eating disorder, are associated with a heightened risk of suicide, presenting a significant challenge for individuals struggling with these conditions, their loved ones, and healthcare providers. Research has consistently demonstrated a strong correlation between eating disorders and suicide risk, underscoring the urgent need for targeted prevention and intervention efforts to address this critical issue.
The Connection Between Eating Disorders and Suicide Risk:
The intricate relationship between eating disorders and suicide risk is a complex interplay of biological, psychological, and social factors, each contributing to the heightened vulnerability of individuals affected by these conditions. Understanding these mechanisms is crucial for developing targeted interventions and support strategies to address the intersecting challenges of eating disorders and suicidal behavior.

1. Co-occurring Mental Health Disorders:
Individuals with eating disorders frequently experience co-occurring mental health conditions, such as depression, anxiety disorders, and substance abuse. These comorbidities often exacerbate the severity of symptoms and contribute to a sense of hopelessness, worthlessness, and despair. For example, depression may intensify feelings of inadequacy and self-criticism, while anxiety disorders may amplify the fear of weight gain or loss of control. Substance abuse, often used as a coping mechanism to numb emotional pain, further complicates the treatment and recovery process, increasing the risk of suicidal ideation and behavior among individuals with eating disorders.
2. Biological Factors:
Studies have suggested that alterations in brain chemistry and neurobiological pathways may contribute to both eating disorders and suicidal behavior. Dysregulation of neurotransmitters such as serotonin, dopamine, and norepinephrine, which play a crucial role in mood regulation and impulse control, has been implicated in the pathophysiology of both conditions. Imbalances in these neurotransmitters may contribute to the dysphoric mood states, impulsivity, and emotional dysregulation observed in individuals with eating disorders, increasing their susceptibility to suicidal ideation and behavior.
3. Psychosocial Stressors:
Individuals with eating disorders often face significant psychosocial stressors that exacerbate their distress and increase their risk of suicidal behavior. These stressors may include interpersonal conflicts, familial dysfunction, peer pressure, academic stress, and societal pressures to conform to unrealistic beauty standards. The pervasive stigma surrounding eating disorders and mental illness further compounds feelings of shame, guilt, and isolation, exacerbating the sense of worthlessness and hopelessness experienced by affected individuals. Body image dissatisfaction, a hallmark feature of eating disorders, is often exacerbated by societal ideals of thinness and attractiveness, contributing to feelings of inadequacy and driving individuals to extreme measures to attain an unattainable standard.
4. Maladaptive Coping Mechanisms:
Individuals with eating disorders often rely on maladaptive coping mechanisms, such as restrictive eating, binge eating, and purging, to manage emotional distress and psychological pain. While these behaviors may provide temporary relief from negative emotions, they ultimately exacerbate feelings of guilt, shame, and self-loathing, perpetuating a vicious cycle of disordered eating and emotional dysregulation. Moreover, these behaviors may serve as a form of self-punishment or self-soothing, reinforcing maladaptive patterns of coping and increasing the risk of suicidal ideation and behavior as a means of escape from intolerable emotional pain.
5. Perceived Lack of Control:
Individuals with eating disorders often experience a pervasive sense of control over their bodies and lives, driven by rigid dietary rules, compulsive exercise habits, and obsessive thoughts about food and weight. However, this perceived sense of control is often illusory and masks underlying feelings of powerlessness and despair. The challenges of recovery, including relinquishing control over food and weight, confronting fears of weight gain, and facing the uncertainties of treatment, may intensify feelings of anxiety and distress, further fueling suicidal ideation and behavior as a means of regaining a sense of control or escaping from perceived failure.
In summary, the connection between eating disorders and suicide risk is multifaceted and influenced by a complex interplay of biological, psychological, and social factors. Recognizing these mechanisms is essential for developing comprehensive interventions and support strategies to address the underlying vulnerabilities and promote recovery and resilience among individuals affected by eating disorders. By addressing the interconnected challenges of mental health, self-esteem, coping mechanisms, and perceived control, we can mitigate the risk of suicidal behavior and improve outcomes for individuals struggling with eating disorders.
Recognizing the Signs of Suicide Risk in Eating Disorders:
Identifying the signs of suicide risk in individuals with eating disorders is paramount for timely intervention and prevention of tragic outcomes. While the symptoms of eating disorders may vary widely among individuals, certain warning signs may indicate an increased risk of suicidal ideation and behavior. By understanding and recognizing these signs, loved ones, caregivers, and healthcare providers can offer support and connect individuals with appropriate resources to address their mental health needs effectively.
1. Expressions of Hopelessness or Despair:
Individuals with eating disorders may express feelings of hopelessness, despair, or a pervasive sense of emptiness. They may articulate a bleak outlook on the future and struggle to envision a path toward recovery. Statements such as “I feel like there’s no way out” or “I can’t see things getting better” may indicate underlying suicidal ideation and warrant immediate attention and support.
2. Increased Social Withdrawal or Isolation:
A significant increase in social withdrawal or isolation may be indicative of escalating distress and emotional turmoil in individuals with eating disorders. They may withdraw from social interactions, avoid gatherings or events involving food, and retreat into isolation as a coping mechanism to manage their internal struggles. Loss of interest in previously enjoyed activities and disengagement from social support networks may signal a heightened risk of suicidal behavior and necessitate intervention.
3. Changes in Eating Behaviors or Body Weight:
Noticeable changes in eating behaviors, such as sudden increases or decreases in food intake, or fluctuations in body weight, may signal underlying distress and exacerbate the risk of suicidal ideation. Individuals with eating disorders may exhibit extreme dietary restriction, binge eating episodes, or purging behaviors as a means of coping with emotional pain or exerting control over their bodies. These behaviors may escalate during periods of heightened stress or emotional upheaval and require immediate intervention to prevent further harm.
4. Persistent Feelings of Guilt or Worthlessness:
Feelings of guilt, worthlessness, and self-loathing are common features of eating disorders and significant risk factors for suicidal ideation. Individuals may harbor intense feelings of shame related to their eating behaviors, body image concerns, or perceived inadequacies. Persistent negative self-talk, self-criticism, and a distorted sense of self-worth may indicate underlying psychological distress and necessitate supportive intervention to address underlying issues and promote self-esteem and self-compassion.
5. Engaging in Self-Harming Behaviors:
Individuals with eating disorders may engage in self-harming behaviors, such as cutting, burning, or scratching, as a maladaptive coping mechanism to manage overwhelming emotions and alleviate psychological pain. These behaviors serve as a means of externalizing internal distress and may escalate in severity as suicidal ideation intensifies. Any indication of self-harm warrants immediate attention and intervention to ensure the individual’s safety and well-being.
6. Making Statements About Feeling Trapped or Having No Reason to Live:
Expressions of feeling trapped, hopeless, or devoid of purpose are significant indicators of suicidal ideation and should be taken seriously. Individuals may express sentiments such as “I can’t go on like this” or “I don’t see the point in living anymore,” signaling a profound sense of despair and emotional pain. These statements require immediate intervention and support to address underlying issues and provide hope and encouragement.
7. Sudden Changes in Mood or Behavior:
Sudden changes in mood or behavior, such as increased agitation, irritability, or impulsivity, may indicate acute distress and escalate the risk of suicidal behavior. Individuals may exhibit mood swings, erratic behavior, or a loss of emotional regulation as they grapple with internal turmoil. These changes may be alarming to those around them and require prompt intervention to ensure their safety and well-being.
8. Giving Away Possessions or Making Final Arrangements:
Individuals contemplating suicide may exhibit preparatory behaviors, such as giving away cherished possessions or making final arrangements, as a way of saying goodbye or tying up loose ends. These actions may be a precursor to suicidal behavior and should be treated as urgent warning signs requiring immediate intervention and support.
If you or someone you know is experiencing suicidal thoughts or behaviors, it’s crucial to seek help immediately. Contacting a mental health professional, crisis hotline, or emergency services can provide immediate support and assistance. Additionally, reaching out to trusted friends, family members, or support groups can offer comfort and guidance during times of crisis. Remember, you are not alone, and help is available. By recognizing the signs of suicide risk and taking proactive steps to intervene, we can save lives and support individuals on their journey toward recovery and healing.
Strategies for Prevention and Intervention:
Preventing suicide among individuals with eating disorders requires a comprehensive and multi-faceted approach that addresses the complex interplay of biological, psychological, and social factors contributing to their vulnerability. By implementing targeted strategies for prevention and intervention, we can reduce the incidence of suicidal ideation and behavior and promote resilience and recovery within this population.
1. Early Identification and Intervention:
Early identification of eating disorders and suicidal ideation is crucial for initiating timely intervention and support. Healthcare providers, educators, family members, and peers should be trained to recognize the warning signs and risk factors associated with these conditions. Screening tools and assessment protocols can aid in identifying individuals at risk, enabling prompt referral to specialized treatment services. Educating the community about the signs and symptoms of eating disorders and suicide risk can help reduce stigma and encourage help-seeking behaviors among those in need.
2. Comprehensive Treatment:
Effective treatment of eating disorders and co-occurring mental health conditions is paramount for reducing suicide risk and promoting long-term recovery. A multidisciplinary approach that addresses the biological, psychological, and social aspects of these disorders is essential. Psychotherapy, such as cognitive-behavioral therapy (CBT), dialectical behavior therapy (DBT), and interpersonal therapy (IPT), can help individuals develop coping skills, challenge distorted thoughts and beliefs, and improve interpersonal functioning. Medication management may be necessary for managing co-occurring mood and anxiety disorders, while nutritional counseling and meal support can address disordered eating behaviors and promote balanced nutrition. Support groups and peer-led initiatives provide valuable peer support and encouragement, fostering a sense of belonging and validation among individuals in treatment.
3. Cultivating Coping Skills:
Empowering individuals with eating disorders to develop healthy coping skills and adaptive strategies for managing stress and emotional distress is essential for reducing the risk of suicidal ideation and behavior. Cognitive-behavioral techniques, such as identifying and challenging negative thought patterns, practicing relaxation exercises, and engaging in problem-solving strategies, can help individuals regulate their emotions and cope effectively with life’s challenges. Dialectical behavior therapy (DBT) emphasizes mindfulness, emotion regulation, interpersonal effectiveness, and distress tolerance skills, providing a comprehensive framework for managing difficult emotions and reducing impulsive behaviors. Mindfulness-based interventions, such as mindfulness-based stress reduction (MBSR) and mindful eating, promote present-moment awareness and nonjudgmental acceptance, enhancing individuals’ ability to cope with triggers and cravings related to their eating disorder.
4. Addressing Body Image Concerns:
Body image dissatisfaction is a significant risk factor for eating disorders and suicide risk, fueled by societal pressures to attain unrealistic beauty standards. Promoting body positivity, self-acceptance, and self-care can help individuals develop a healthier relationship with their bodies and reduce the impact of societal pressures on their self-esteem and well-being. Encouraging self-compassion and challenging perfectionistic beliefs can foster a sense of worthiness and acceptance, empowering individuals to embrace their bodies and focus on their strengths and values beyond appearance. Education initiatives aimed at challenging stereotypes and promoting diversity and inclusivity can help shift societal attitudes toward body image and reduce the prevalence of weight stigma and discrimination.
5. Creating Supportive Environments:
Creating supportive environments that foster empathy, understanding, and acceptance is essential for promoting mental health and well-being among individuals with eating disorders. Peer support groups, online communities, and advocacy organizations provide valuable opportunities for individuals to connect with others who share similar experiences, validate their feelings, and offer mutual support and encouragement. Peer-led initiatives, such as recovery-focused events, art therapy workshops, and body-positive campaigns, promote empowerment and resilience within the community. Schools, workplaces, and healthcare settings can implement policies and practices that prioritize mental health and create inclusive environments free from stigma and discrimination. Training programs for educators, healthcare providers, and community leaders can raise awareness about eating disorders and suicide risk, improve access to resources and support services, and enhance the quality of care provided to individuals in need.
In summary, strategies for preventing suicide among individuals with eating disorders encompass early identification and intervention, comprehensive treatment approaches, cultivation of coping skills, addressing body image concerns, and creating supportive environments. By addressing the underlying risk factors and promoting resilience and recovery, we can reduce the incidence of suicidal ideation and behavior and support individuals on their journey toward healing and well-being. Collaborative efforts across sectors are essential for implementing these strategies effectively and creating a culture of care and compassion for those affected by eating disorders.
Conclusion:
In conclusion, the connection between eating disorders and suicide risk is a critical and multifaceted issue that demands attention and action from all sectors of society. Eating disorders not only pose significant physical health risks but also increase the likelihood of suicidal ideation and behavior among affected individuals. Factors such as co-occurring mental health conditions, biological vulnerabilities, psychosocial stressors, maladaptive coping mechanisms, and a perceived lack of control contribute to the heightened suicide risk in individuals with eating disorders. Recognizing the signs of suicide risk in this population is crucial for early intervention and prevention efforts. Strategies for prevention and intervention include early identification and intervention, comprehensive treatment approaches, cultivating coping skills, addressing body image concerns, and creating supportive environments. By implementing these strategies and prioritizing mental health awareness and support, we can reduce the incidence of suicide and promote recovery and resilience among individuals affected by eating disorders.
2) FAQs with Answers:
Q1: Are eating disorders and suicide risk closely linked?
A1: Yes, research has shown a strong association between eating disorders and suicide risk, highlighting the need for targeted prevention and intervention efforts.
Q2: What are some warning signs of suicide risk in individuals with eating disorders?
A2: Warning signs may include expressions of hopelessness, social withdrawal, changes in eating behaviors or body weight, persistent feelings of guilt or worthlessness, and engaging in self-harming behaviors.
Q3: How can I help someone with an eating disorder who is experiencing suicidal thoughts?
A3: Encourage them to seek professional help, offer support and understanding, and connect them with resources such as hotlines, support groups, and treatment services.
Q4: What are some effective treatment options for individuals with eating disorders and suicidal ideation?
A4: Comprehensive treatment approaches may include psychotherapy, medication management, nutritional counseling, and support groups tailored to address both eating disorder symptoms and underlying mental health issues.
Q5: What role do societal pressures and body image concerns play in the development of eating disorders and suicide risk?
A5: Societal pressures to conform to unrealistic beauty standards and body image dissatisfaction can contribute to the development of eating disorders and increase the risk of suicide among affected individuals.
Your article helped me a lot, is there any more related content? Thanks!
Your point of view caught my eye and was very interesting. Thanks. I have a question for you.
Can you be more specific about the content of your article? After reading it, I still have some doubts. Hope you can help me.
Your article helped me a lot, is there any more related content? Thanks!
Your article helped me a lot, is there any more related content? Thanks!
Thanks for sharing. I read many of your blog posts, cool, your blog is very good.
Your article helped me a lot, is there any more related content? Thanks!
Thank you for your sharing. I am worried that I lack creative ideas. It is your article that makes me full of hope. Thank you. But, I have a question, can you help me?
Thanks for sharing. I read many of your blog posts, cool, your blog is very good.
I don’t think the title of your article matches the content lol. Just kidding, mainly because I had some doubts after reading the article.
Can you be more specific about the content of your article? After reading it, I still have some doubts. Hope you can help me.
Can you be more specific about the content of your article? After reading it, I still have some doubts. Hope you can help me.
Can you be more specific about the content of your article? After reading it, I still have some doubts. Hope you can help me. https://www.binance.info/zh-CN/register?ref=VDVEQ78S
Can you be more specific about the content of your article? After reading it, I still have some doubts. Hope you can help me.
Blog được xây dựng với mục tiêu chia sẻ thông tin hữu ích, cập nhật kiến thức đa dạng và mang đến góc nhìn khách quan cho bạn đọc. Nội dung tập trung vào việc tổng hợp, phân tích và truyền tải một cách minh bạch – dễ hiểu, giúp bạn tiếp cận nguồn thông tin chất lượng trong nhiều lĩnh vực.
Thank you for your sharing. I am worried that I lack creative ideas. It is your article that makes me full of hope. Thank you. But, I have a question, can you help me? https://www.binance.info/ES_la/register?ref=T7KCZASX
Thank you for your sharing. I am worried that I lack creative ideas. It is your article that makes me full of hope. Thank you. But, I have a question, can you help me? https://www.binance.info/el/register-person?ref=IQY5TET4
Can you be more specific about the content of your article? After reading it, I still have some doubts. Hope you can help me.
Your point of view caught my eye and was very interesting. Thanks. I have a question for you.
Thanks for sharing. I read many of your blog posts, cool, your blog is very good.
Reading your article helped me a lot and I agree with you. But I still have some doubts, can you clarify for me? I’ll keep an eye out for your answers.
Sứ mệnh của tôi là giúp doanh nghiệp chuyển mình, bằng cách ứng dụng công nghệ tự động hóa.
Chúng tôi tin rằng sẽ mở ra tương lai mới — nơi con người và công nghệ cùng tồn tại.
Đội ngũ chuyên gia công nghệ nhiệt huyết với sáng tạo công nghệ nhằm mang lại giá trị bền vững cho doanh nghiệp.
#CôngNghệ #ChuyểnĐổiSố #Innovation #TechLife #DigitalEra
Sứ mệnh của tôi là kết nối công nghệ với cuộc sống thực, thông qua ứng dụng công nghệ tự động hóa.
#CôngNghệ #ChuyểnĐổiSố #Innovation #TechLife #DigitalEra
Với khả năng thích ứng nhanh, team chủ động cập nhật xu hướng công nghệ mới nhất để xây dựng hệ sinh thái số.
#CôngNghệ #ChuyểnĐổiSố #Innovation #TechLife #DigitalEra
Chúng tôi nhiệt huyết với sáng tạo công nghệ nhằm nâng cao trải nghiệm người dùng.
Với nền tảng chuyên môn vững chắc, team không ngừng phát triển xu hướng công nghệ mới nhất để thúc đẩy chuyển đổi số.
Sự phát triển của công nghệ sẽ tạo nên đột phá cho thế hệ tiếp theo — nơi trí tuệ nhân tạo và cảm xúc con người song hành.
Sức mạnh của đổi mới sáng tạo sẽ tạo nên đột phá cho thế hệ tiếp theo — nơi con người và công nghệ song hành.
Chúng tôi tin rằng sẽ mở ra tương lai mới — nơi con người và công nghệ phát triển hài hòa.
Thank you for your sharing. I am worried that I lack creative ideas. It is your article that makes me full of hope. Thank you. But, I have a question, can you help me? https://www.binance.info/zh-TC/register-person?ref=VDVEQ78S
With a solid professional foundation, we actively update the latest technology trends to build a digital ecosystem.
I believe will create breakthroughs for the next generation — where humans and technology move forward together.
#Technology #DigitalTransformation #Innovation #TechLife #DigitalEra
#Technology #DigitalTransformation #Innovation #TechLife #DigitalEra
With a pioneering mindset, we continuously research AI, IoT, Blockchain, and Cloud solutions to expand creative capabilities.
The power of innovation will create breakthroughs for the next generation — where data and creativity move forward together.
#Technology #DigitalTransformation #Innovation #TechLife #DigitalEra
The mission of mine is to create intelligent value, by providing optimal consulting solutions.
The evolution of technology will open a new future — where artificial intelligence and human emotions move forward together.
With a solid professional foundation, we actively update the latest technology trends to expand creative capabilities.
We believe will create breakthroughs for the next generation — where humans and technology develop in harmony.
With strong adaptability, we constantly develop the latest technology trends to build a digital ecosystem.
#Technology #DigitalTransformation #Innovation #TechLife #DigitalEra
Thanks for sharing. I read many of your blog posts, cool, your blog is very good.
I don’t think the title of your article matches the content lol. Just kidding, mainly because I had some doubts after reading the article.
Buying a stake in the company won’t help Star’s precarious financial position. If he had been lined up or approached by the Star board as part of the rescue attempt, the company would need to have disclosed any deal or association. Mr Costello said it was more in the public interest to let the facility be sold off for “a shopping centre” than to prop up a failing casino with taxpayers’ money. He said the public could have “no confidence” in a casino owner that had failed to disclose business dealings with organised crime figures.
Really, it’s the ability to come and go as they like that appeals most to people. A lot of people download Tubi because it’s similar to what they already know. Weird, wonderful and forgotten movies can be found here on Tubi. Sometimes, a long day just leaves you wishing for something light to watch or when you’re watching with friends, they won’t all want to see the same thing.
References:
https://blackcoin.co/ufo9-casino-your-place-to-play-your-way/
online slots uk paypal
References:
slonec.com
casino avec paypal
References:
https://www.busforsale.ae/profile/zulmaheane1037
casino mit paypal
References:
dodo00.dothome.co.kr
paypal casinos online that accept
References:
https://ezworkers.com/employer/paypal-casinos-best-online-casinos-that-accept-paypal/
Wenn Sie im Internet um echtes Geld spielen, ist die Sicherheit und Fairness des Spiels der wichtigste Faktor. Und wenn Sie besonders gerne Boni oder Slot-Turniere spielen, ist HitnSpin der richtige Ort für Sie. Wer weiterspielen möchte, benötigt spätestens dann Echtgeld, wenn die Free Spins und die Gewinne daraus verbraucht sind. Um die 50 Freispiele von Hit’n’Spin zu erhalten, ist eine vorherige Anmeldung erforderlich.
Das Casino bietet ein breites Spektrum an Spielen von führenden Softwareanbietern, die ein vielfältiges und ansprechendes Sortiment für seine Kunden gewährleisten. HitNSpin 🔥 arbeitet unter einer Lizenz der Regierung von Curacao, die ein grundlegendes Maß an Vertrauenswürdigkeit bietet. Die HitNSpin Casino-App bietet ein modernes und optisch ansprechendes Design mit einer anwenderfreundlichen Benutzeroberfläche.
References:
https://s3.amazonaws.com/new-casino/n1%20casino.html
References:
Women anavar cycle before after
References:
https://morphomics.science/wiki/Anavar_Before_and_After_Results
References:
Slot machine jammer
References:
https://timeoftheworld.date/wiki/WD40_Casino
References:
Roulette odds
References:
https://atavi.com/share/xnibgwz9yyav
closest you fit
References:
https://urlscan.io/result/019bc0b0-4df9-75c0-879f-32550b16b5fa/
References:
Female before and after anavar
References:
https://apunto.it/user/profile/555914
References:
Transformation anavar female before and after
References:
https://funsilo.date/wiki/Oxandrolon_Anavar_Einsatz_Wirkung_im_Sport
References:
Anavar cycle results before and after pics
References:
https://trolle-mcneil.thoughtlanes.net/anavar-cure-cycle-combinaisons-calendrier-et-faq
can steroids help you lose weight
References:
https://pattern-wiki.win/wiki/9_metodi_per_aumentare_i_livelli_di_testosterone_in_modo_naturale
anabolic steroids for sale usa
References:
https://securityholes.science/wiki/Natrliche_Appetitzgler_Welche_Lebensmittel_helfen_wirklich
%random_anchor_text%
References:
https://telegra.ph/Quale-farmaco-per-dimagrire-01-20
References:
Rabbi alon anava before and after
References:
https://bookmarkstore.download/story.php?title=anavar-before-and-after-effects-results-and-risks
%random_anchor_text%
References:
https://www.askocloud.com/index.php/user/capthrill04
metabolic vs anabolic
References:
https://coolpot.stream/story.php?title=come-acquistare-gel-testosterone-on-line
lean mass cycle
References:
https://urlscan.io/result/019bce09-be31-719c-9d53-631b12cc69ec/
References:
How slot machines work
References:
https://bookmarkingworld.review/story.php?title=bewertungen-zu-candy-ai-lesen-sie-kundenbewertungen-zu-candy-ai-eu
References:
Casino club
References:
https://socialbookmark.stream/story.php?title=online-casino-willkommensbonus-mit-einzahlung-2026-%EF%B8%8F-legal
References:
Euroking casino
References:
https://bookmarkingworld.review/story.php?title=candy-crush-saga-level-91-92-93-94-95-96-97-98-99-100-loesung
References:
Slot marsepeinstein
References:
https://www.blurb.com/user/budgetpasta1
References:
Video poker jacks or better
References:
https://justbookmark.win/story.php?title=slot-games-like-candy-crush-you-can-find-at-online-casinos
References:
Emploi restomontreal
References:
https://pad.stuve.uni-ulm.de/s/Q6np6aslh
References:
Hard rock casino northfield ohio
References:
http://stroyrem-master.ru/user/beadjudge00/
References:
Casino games online
References:
https://justbookmark.win/story.php?title=recambio-deposito-secadora-candy-hoover-otsein-40008542
References:
Latest casino bonuses
References:
https://lpstandup.com/members/drivegolf3/activity/33287/
References:
Lucky play casino
References:
https://molchanovonews.ru/user/formatniece0/
References:
William hill android app
References:
https://sciencewiki.science/wiki/Candy_Corner_machine_sous_Pragmatic_Play_Jouez_gratuitement
References:
Moncton new brunswick
References:
https://may22.ru/user/animemint0/
%random_anchor_text%
References:
https://pad.karuka.tech/s/Ng40S-kXy
%random_anchor_text%
References:
https://humanlove.stream/wiki/Acquista_Clenbuterolo_online_in_Italia_senza_ricetta
purchasing anabolic steroids online
References:
https://kirkegaard-roberts-2.technetbloggers.de/androtiv-gel-a-la-testosterone-40-sachets-unidoses
i want to buy steroids
References:
https://pattern-wiki.win/wiki/Buy_Clenbuterol_Tablets_Online_for_Sale
%random_anchor_text%
References:
https://pattern-wiki.win/wiki/Wie_Testosteron_steigern_Urologe_erklrt_was_Mnnern_wirklich_hilft
%random_anchor_text%
References:
https://nephila.org/members/crocusmouse2/activity/1127788/
bodybuilders after steroids
References:
https://bookmarks4.men/story.php?title=5-htp-besserer-schlaf-easy-abnehmen-das-beweisen-studien
best steroid source
References:
https://dentepic.toothaidschool.com/members/gongpuppy5/activity/18272/
what is the best steroid stack
References:
https://morphomics.science/wiki/Comprar_Winstrol_Stanozolol_Online_al_Mejor_Precio_en_Espaa
the best legal steroids on the market
References:
https://www.pathofthesage.com/members/springfender09/activity/742310/
steroids pills for bodybuilding
References:
https://scientific-programs.science/wiki/What_Drugs_Will_Make_You_Lose_Weight_Effective_Safe_Proven
References:
Atlantis casino bahamas
References:
https://socialbookmark.stream/story.php?title=candy96-online-casino-australia-100-welcome-bonus-and-other-bonuses
References:
Bert and ernie casino
References:
http://cqr3d.ru/user/fontaction8/
References:
Langley casino
References:
https://gaiaathome.eu/gaiaathome/show_user.php?userid=1826354
References:
Aristocrat slot machines
References:
https://humanlove.stream/wiki/Candy96_Reviews
References:
Slot games for android
References:
https://buchanan-mullins-2.technetbloggers.de/australia-top-online-pokies-casino-entertainment-hub
References:
Cinema casino bagnols sur ceze
References:
https://able2know.org/user/yogurtring92/
References:
William hill app android
References:
https://gaiaathome.eu/gaiaathome/show_user.php?userid=1826416
References:
Campione d italia casino
References:
https://forum.issabel.org/u/cloudeggnog4
References:
Wynn casino las vegas
References:
https://graph.org/CANDY-JACKPOT-SLOT-MACHINE-01-26
References:
Online roulette play roulette and receive $1500
References:
https://googlino.com/members/patchcycle79/activity/585441/
References:
No download casino
References:
https://cameradb.review/wiki/Online_Casino_De_Beste_Online_Casinos_van_Nederland_voor_2025
References:
Roxy casino
References:
https://gpsites.stream/story.php?title=a-big-candy-casino-promo-codes-2026-100-no-deposit-350-bonus
References:
Cleveland casino
References:
https://saveyoursite.date/story.php?title=win-instantly-with-real-money-online
References:
Casino odds
References:
https://pediascape.science/wiki/Candy96_Australia_18_NoDeposit_Fast_OSKO_PayID_Cashouts_VIP_Perks_2025
after stopping steroids
References:
https://prpack.ru/user/hoodharp7/
what is the best legal steroid on the market
References:
http://hikvisiondb.webcam/index.php?title=cliffordsargent6903
best muscle stacks 2015
References:
https://menwiki.men/wiki/A_cosa_serve_il_testosterone_nel_body_building
where to get illegal steroids
References:
https://ondashboard.win/story.php?title=dianabol-online-kaufen-top-preis-rezeptfrei-in-deutschland
Thank you for your sharing. I am worried that I lack creative ideas. It is your article that makes me full of hope. Thank you. But, I have a question, can you help me? https://accounts.binance.com/sv/register-person?ref=GQ1JXNRE
References:
Game dua oto
References:
https://cameradb.review/wiki/Online_Casino_Bonus_2026_Die_wirklich_besten_Angebote_im_Vergleich_fr_Deutschland_sterreich_und_die_Schweiz
References:
Roulette online
References:
https://medibang.com/author/27669004/
References:
Chumash casino
References:
https://doodleordie.com/profile/braswellpollock7721
References:
Treasure island casino mn
References:
http://celebratebro.in/birthdays-in-bangalore/index.php?qa=user&qa_1=personcarbon1
Live streams https://golvar.com.az/ and live matches online, including the latest football schedule for today. Follow games in real time, find out dates, start times, and key events of football tournaments.
References:
Blackjack basic strategy
References:
https://rentry.co/m93a2txx
References:
Game chuzzle
References:
https://graph.org/PayID-Deposit-Casino-Australia–Top-Sites-with-Min-Deposit-02-01
заклепка вытяжная отверстие заклепка вытяжная
Сейчас работает кракен маркет зеркало krab1.cc для быстрого входа на площадку
References:
St joe frontier casino
References:
https://chessdatabase.science/wiki/Osko_by_BPAY_Ways_to_Bank
References:
Pittsburgh casino
References:
https://www.google.ci/url?q=https://www.facebook.com/people/Winz-io-casino/61585762127473/
References:
Potawatomi casino milwaukee
References:
http://okprint.kz/user/cloudcase47/
Thank you for your sharing. I am worried that I lack creative ideas. It is your article that makes me full of hope. Thank you. But, I have a question, can you help me?
дома коттеджи дизайн фото дизайн загородных домов и коттеджей
дизайны комнат в квартире дизайн проект 2 х комнатной
best non steroid supplement
References:
https://web.ggather.com/drysex56/
reddit steroids before and after
References:
https://lovewiki.faith/wiki/The_Largest_Online_Healthcare_Clinic_in_North_America_Affordable_Pricing_Enjoy_Increased_Energy_Focus
are steroids legal in the nba
References:
https://hikvisiondb.webcam/wiki/Buy_10_mL_Vial
подключение полотенцесушителя купить полотенцесушитель
References:
Paypal casinos
References:
https://dokuwiki.stream/wiki/Top_PayID_Casinos_Australia_2026_Instant_Pokies_Deposits
I would like to thnkx for the efforts you have put in writing this web site. I’m hoping the same high-grade web site post from you in the upcoming also. In fact your creative writing abilities has inspired me to get my own site now. Actually the blogging is spreading its wings fast. Your write up is a great example of it.
before and after steroid cycle
References:
https://bookmarkspot.win/story.php?title=8-brands-generics-human-growth-hormone-hgh-injections
anabolic steroids slang names
References:
https://p.mobile9.com/donkeydrum5/
what is steroids good for
References:
https://gpsites.win/story.php?title=trenbolone-acetate-an-overview
arnold schwarzenegger on steroids
References:
https://trade-britanica.trade/wiki/Anavar_Ist_dieses_anabole_Steroid_sicher_zu_verwenden
best supplement stack for mass
References:
https://onlinevetjobs.com/author/storywhale0/
reasons to take steroids
References:
https://skitterphoto.com/photographers/2218050/sherman-ahmed
most popular steroids for bodybuilding
References:
https://socialbookmark.stream/story.php?title=trenbolone-review-is-this-steroid-worth-the-risk
best cutting stack
References:
https://onlinevetjobs.com/author/coursespear0/
best steroids without side effects
References:
https://funsilo.date/wiki/Mercado_Libre
safe steroids for bodybuilding
References:
https://wifidb.science/wiki/Acheter_du_Trenbolone_Injectable_Trenbolone_Injection_en_vente_sur_Lecoq_to
illegal pre workout supplements
References:
https://bbs.pku.edu.cn/v2/jump-to.php?url=https://wisdom.edu.al/wp-includes/pgs/?where_to_buy_clenbuterol__3.html
deca durabolin before after
References:
https://dreevoo.com/profile.php?pid=1063645
what is the best muscle building supplement at gnc
References:
https://onlinevetjobs.com/author/nameskiing64/
bulk steroid cycle
References:
https://www.instapaper.com/p/17441049
legal anabolic stacks
References:
https://socialisted.org/market/index.php?page=user&action=pub_profile&id=316029
legal steroids at gnc
References:
https://mercado-macias-3.hubstack.net/exp-c3-a9riences-et-avis-sur-les-capsules-shape-voici-comment-vous-pouvez-perdre-du-poids-avec-les-capsules-pour-le-soutien-du-m-c3-a9tabolisme
anabolic steroid review
References:
http://historydb.date/index.php?title=sejersengamble3711
steroids negative effects
References:
https://historydb.date/wiki/Anavar_The_Good_The_Bad_and_The_Ugly
steroids to build muscle fast
References:
https://bookmarking.win/story.php?title=anavar-bodybuilding-supplement-for-muscle-strength
jay cutler steroids cycle
References:
https://telegra.ph/Bestellen-Sie-ANAVAR-UNIGEN-in-der-Deutschland-online-um-102-00-von-einer-Online-Apotheke-02-06
best cutting supplement stack
References:
http://stroyrem-master.ru/user/pajamasalary0/
bodybuilder steroid
References:
https://bookmarks4.men/story.php?title=warnung-appetitzuegler-test-2022-10-hersteller-im-vergleich
gnc supplements for muscle growth
References:
https://bryant-case.federatedjournals.com/comment-acheter-des-pilules-ou-comprimes-davortement-surs-et-efficaces-1770378369
anabolic steroid cost
References:
https://lovewiki.faith/wiki/Anavar_10mg_50_tabs_Buy_Online_USA
post steroid cycle therapy
References:
https://www.youtube.com/redirect?q=https://thehollywoodtrainer.com/wp-content/pgs/?pills_to_boost_testosterone.html
different steroids
References:
https://graph.org/Anavar-Testbericht-Wirkungen-und-Besonderheiten-des-anabolen-Steroids-02-06
Its like you read my mind! You seem to know so much about this, like you wrote the book in it or something. I think that you could do with some pics to drive the message home a little bit, but other than that, this is fantastic blog. An excellent read. I’ll definitely be back.
dianabol 10
References:
https://graph.org/Anavar-Ist-dieses-anabole-Steroid-sicher-zu-verwenden-02-06
penis enlargement hormone
References:
https://timeoftheworld.date/wiki/3_mdicaments_pour_perdre_du_poids_au_Canada
where to buy anadrol
References:
https://dodd-yu-2.mdwrite.net/anavar-10mg-100-tabs-1770376461
define androgenic
References:
https://www.sommer-architekt-warstein.de/VPB-Expertenrat;focus=TKOMSI_com_cm4all_wdn_Flatpress_22800952&frame=TKOMSI_com_cm4all_wdn_Flatpress_22800952?x=entry:entry210615-143953%3Bcomments:1
casino drive lagny
References:
https://www.rabenwind.de/rabenwind-blog;focus=TKOMSI_com_cm4all_wdn_Flatpress_20842902&path=&frame=?x=entry:entry201116-195228%3Bcomments:1
manoir de beauregard
References:
https://www.fcla.de/index.php/;focus=STRATP_com_cm4all_wdn_Flatpress_38266970&frame=STRATP_com_cm4all_wdn_Flatpress_38266970?x=entry:entry230305-171041%3Bcomments:1
bicycle club casino
References:
https://500px.com/p/hesselbergxsumccarthy
winning at blackjack
References:
https://livebookmark.stream/story.php?title=serioese-online-casino-top-13-casinos-fuer-oesterreich-2026-graz
station casinos las vegas
References:
http://uchkombinat.com.ua/user/beechroad3/
brisbane casino
References:
https://kanban.xsitepool.tu-freiberg.de/s/r1gUgbuu-l
casino slots play for fun
References:
https://sibze.ru/index.php?subaction=userinfo&user=flagguilty7
onlinegamer
References:
https://dreevoo.com/profile.php?pid=1160537
monkey money
References:
https://zenwriting.net/firedesire81/mega-medusa-bonus-codes-mega-medusa-casino-free-chip
casino slots
References:
https://etuitionking.net/forums/users/playoyster55/
wheeling casino
References:
http://ezproxy.cityu.edu.hk/login?url=https://free100pokiesnodeposit.blackcoin.co
club online
References:
https://lundgren-moon.federatedjournals.com/free-100-pokies-no-deposit-sign-up-bonus-australia-in-2025
fairmont charlevoix
References:
https://king-bookmark.stream/story.php?title=free-100-pokies-no-deposit-sign-up-bonus-2025
casino online roulette
References:
https://adsintro.com/index.php?page=user&action=pub_profile&id=831840
kansas casinos
References:
http://stroyrem-master.ru/user/helenlip4/
ameristar casino vicksburg ms
References:
https://sabarinews.com/2025/01/03/36554/
solstafir
References:
https://mensvault.men/story.php?title=registriere-dein-spielerkonto-bei-instant-casino
learn to play craps
References:
https://cattletrailers.com.au/author/davidmarble1/
quasar games
References:
https://school-of-safety-russia.ru/user/bushwhorl8/
blackjack trainer
References:
https://skitterphoto.com/photographers/2363590/webb-gauthier
inter casino
References:
https://nhadat24.org/author/cloudarrow8
super jackpot
References:
https://mapleprimes.com/users/turkeygate7
premier casino
References:
https://panoptikon.org/user/rewardporch1/
video poker download
References:
https://graph.org/iPhone-Top-Games–Apps-02-23
nouveau brunswick
References:
http://xn--l1ae1d.xn--b1agalyeon.xn--80adxhks/user/grouptalk0/
grand eagle casino
References:
https://bbs.pku.edu.cn/v2/jump-to.php?url=https://galaxy96casino.blackcoin.co
noble casino
References:
https://skitterphoto.com/photographers/2367809/nikolajsen-mcclellan
holland casino scheveningen
References:
https://coolpot.stream/story.php?title=online-play-environment-for-australia
slot machine deluxe
References:
https://freebookmarkstore.win/story.php?title=online-play-environment-for-australia
online roulette strategy
References:
https://md.ctdo.de/s/LkeUZfZsyE
good game sites
References:
https://timeoftheworld.date/wiki/E_wallet_casino_list_for_Australia
Thank you for your sharing. I am worried that I lack creative ideas. It is your article that makes me full of hope. Thank you. But, I have a question, can you help me? https://accounts.binance.info/es-AR/register-person?ref=UT2YTZSU
casino listings
References:
https://kivureporter.net/beni-liccn-et-lautorite-couturiere-de-bapakombe-saccordent-sur-un-reglement-pacifique-du-conflit-foncier-autour-du-pnvi/
making steroids
References:
https://skitterphoto.com/photographers/2373866/moreno-olesen
%random_anchor_text%
References:
http://stroyrem-master.ru/user/helenvessel3/
casino world challenge
References:
https://homedecorideas24.co.uk/decoration-pink-chinchilla-pattern-tw2gte-the-ultimate-guide-to-this-luxurious-design-trend/
anabolic steroids pros and cons
References:
https://escatter11.fullerton.edu/nfs/show_user.php?userid=9593725
ameristar casino st louis
References:
https://www.familygreenberg.com/index2.php/2012/01/through-the-filters-if-all-the-debates-were-like-this-id-watch-them/
%random_anchor_text%
References:
https://cineblog01.rest/user/detailpolice6/
winning at roulette
References:
https://www.swinarski.org/page1.php?messagepage=70807&messagePage=
%random_anchor_text%
References:
https://lovewiki.faith/wiki/Anavar_kaufen_Wo_und_wie_legal_erwerben
steroids meaning and side effects
References:
http://ezproxy.cityu.edu.hk/login?url=https://hcgbeilstein.de/media/com_articles/anavar_kaufen_4.html
st louis casinos
References:
http://www.upendogroup.ngdafrica.com/spip.php?article56
%random_anchor_text%
References:
https://shenasname.ir/ask/user/batbush9
black jack davey
References:
https://chilipilli.com/beautiful-lady-hookup/
%random_anchor_text%
References:
https://actualites.cava.tn/user/liftlisa1/
hgh vs steroids bodybuilding
References:
https://g.clicgo.ru/user/garlicisland0/
tren results before and after
References:
https://may22.ru/user/degreespoon9/
casino zandvoort
References:
https://sabarinews.com/2026/02/06/51915/
%random_anchor_text%
References:
https://mueller-cooley-2.blogbright.net/anavar-kur-plan-dosierung-und-kombinationen-1772025864
online games play
References:
https://rushbrainhomes.com/advanced-amino-formula-after-age-of-40/
%random_anchor_text%
References:
https://apunto.it/user/profile/678031
erie pa casino
References:
https://forum.karnex.in/question/recovery-your-stolen-crypto-btc-usdt-eth-with-the-help-of-trace-hackers-crypto-recovery-447355702876-2/
wizard of odds blackjack
References:
http://schlatthof.net/togo-reise-maerz-2023/die-maerz-reise-2023-geht-los/
alice springs casino
References:
http://schlatthof.net/togo-reise-november-2023/es-geht-gleich-in-die-vollen-uns-erster-tag-in-togo/
jacks or better
References:
https://vietlinklogistics.com/cac-tuyen-dac-biet/chuyen-phat-nhanh-tu-viet-nam-sang-singapore.html
casino night fundraiser
References:
https://marketmed.kz/news/spaysovaya-zavisimost-myetody-lyechyeniya/
silver reef casino
References:
https://fashionandtravelreporter.com/buzios-os-principais-pontos-turisticos-da-cidade/
cairns casino
References:
https://wspomozycielka-lodz.pl/?p=907
turning stone casino
References:
https://forum.karnex.in/?show=answers
usa online casinos
References:
https://legal-immobilier.fr/optimiser-la-rentabilite-de-son-bien-locatif/
morongo casino
References:
https://watbosa.ac.th/question/csfhhgggg/
green valley ranch casino
References:
https://raskrussia.ru/blog/artem-galunin-lyzhnoe-dvoebore/
casino online argentina
References:
https://vivek-desai.com/shortcodes/image-teasers/
casino rewards
References:
https://royaltech.ng/2024/04/25/the-evolution-of-smart-home-electrical-systems-for-everyone/
online casino schweiz
References:
https://www.realitateavalceana.ro/bilan%c8%9bul-ipj-valcea-pe-2025-obiective-pentru-2026/
black jack gum
References:
https://shkolnaiapora.ru/question/podstav-slova-v-slovometr
santa barbara casino
References:
https://raskrussia.ru/blog/vopros-vozvrashcheniya-rossiyskikh-prygunov-na-lyzhakh-s-tramplina-i-dvoebortsev-na-mezhdunarodnye-starty-ostaetsya-otkrytym/
solstafir
References:
https://www.bonbini-na-curacao.nl/cropped-seru-coral-logo-5-png/
simslots
References:
https://watbosa.ac.th/question/csfgnhiuu/
real money slots
References:
https://bitpoll.de/poll/OgHDL7tOy7/
golden nugget las vegas nv
References:
https://cpdbouvxc3m7.blog.fc2.com/blog-entry-295.html
peppermill casino
References:
https://animallovergifts.com/loveyourpetday/
new mexico casinos
References:
https://cpdbouvxc3m7.blog.fc2.com/blog-entry-376.html
neteller india
References:
https://bobojesen.com/aenean-vulputate-eleifend-tellus-aenean-leo-ligula/
3d roulette
References:
https://magiamgia.blog.fc2.com/blog-entry-48494.html
Thank you for your sharing. I am worried that I lack creative ideas. It is your article that makes me full of hope. Thank you. But, I have a question, can you help me?
For those seeking an exceptional online gaming experience, us.com](https://maxispin.us.com/) stands out as a premier destination. At Maxispin Casino, players can enjoy a vast array of pokies, table games, and other thrilling options, all accessible in both demo and real-money modes. The casino offers attractive bonuses, including free spins and a generous welcome offer, along with cashback promotions and engaging tournaments. To ensure a seamless experience, Maxispin provides various payment methods, efficient withdrawal processes, and reliable customer support through live chat. Security is a top priority, with robust safety measures and a strong focus on responsible gambling tools. Players can easily navigate the site, with detailed guides on account creation, verification, and payment methods. Whether you’re interested in high RTP slots, hold and win pokies, or the latest slot releases, Maxispin Casino delivers a user-friendly and secure platform. Explore their terms and conditions, read reviews, and discover why many consider Maxispin a legitimate and trustworthy choice in Australia.
The platform is user-friendly, making it accessible to everyone.
**Features of MaxiSpin.us.com**
Additionally, the platform offers a built-in editor for making real-time edits to achieve optimal results.
**Benefits of Using MaxiSpin.us.com**
Businesses benefit greatly from MaxiSpin.us.com as it streamlines the process of creating content.
negative effect definition
References:
https://shapiro-stage-3.hubstack.net/top-10-des-sites-pour-acheter-de-la-testosterone-testosterone-steroids-com
steroids winstrol
References:
https://travelersqa.com/user/gardenraven9
steroid use before and after
References:
https://quaildonald3.werite.net/guide-essentiel-pour-lachat-de-testosterone-securise
best steroid
References:
https://hikvisiondb.webcam/wiki/Sopharma_Clenbuterol_20mcg_Tablets_Fat_Burning_Cutting_Support
anabolic masster gnc
References:
https://molchanovonews.ru/user/foxonion6/
anabolic products
References:
https://skitterphoto.com/photographers/2379580/rodriguez-wynn
cass martin steroids
References:
http://kriminal-ohlyad.com.ua/user/wayyew2/
best gnc supplements to get ripped
References:
http://stroyrem-master.ru/user/summercarp1/
best female supplement stacks
References:
https://output.jsbin.com/rehadawasi/
is short term prednisone use dangerous
References:
https://graph.org/40-mcg-Fat-Burner-Tablets-USA-03-02
the best cutting steroid
References:
https://bom.so/kj8U3w
Hey! I know this is kinda off topic however I’d figured I’d ask. Would you be interested in exchanging links or maybe guest authoring a blog article or vice-versa? My site addresses a lot of the same topics as yours and I feel we could greatly benefit from each other. If you might be interested feel free to send me an email. I look forward to hearing from you! Excellent blog by the way!
bodybuilding steroids forum
References:
https://raindrop.io/wishnose1/pollockbarker3601-67636133
Discover the thrill of real-money live casino action at top casino software, where you can enjoy live dealers, top software providers, and exclusive promotions.
Regular updates keep maxispin-au.com aligned with technological advances and user feedback.